Genetically Proxied Diurnal Preference, Sleep Timing, and Risk of Major Depressive Disorder
Importance: Morning diurnal preference is associated with reduced risk of major depressive disorder (MDD); however, causality in this association is uncertain.
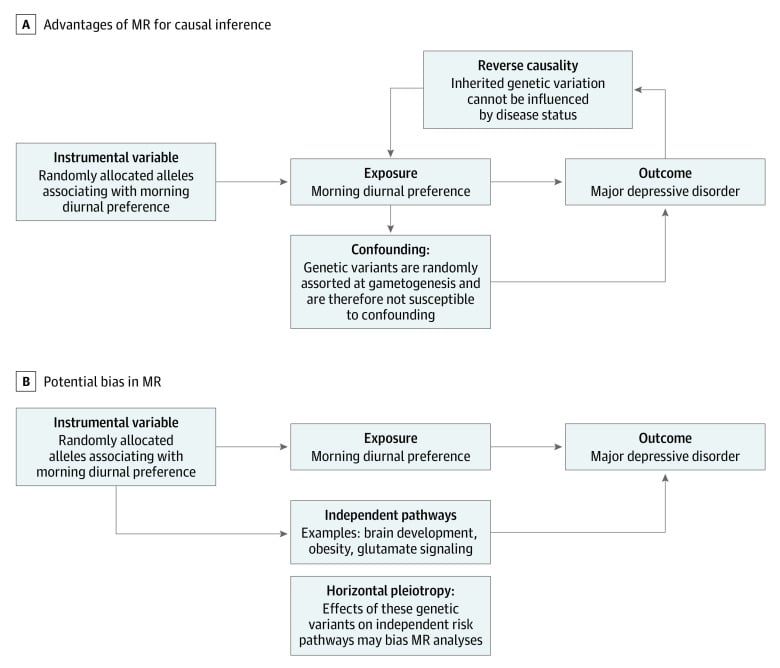
Objective: To examine the association of genetically proxied morning diurnal preference with depression risk using mendelian randomization.
Design, setting, and participants: This 2-sample mendelian randomization study used summary-level genetic associations with diurnal preference and MDD. Up to 340 genetic loci associated with diurnal preference in a meta-analysis of the UK Biobank and 23andMe cohorts were considered as genetic proxies for diurnal preference. The effect size of these variants was scaled using genetic associations with accelerometer-based measurement of sleep midpoint. Genetic associations with MDD were obtained from a meta-analysis of genome-wide association studies data from the Psychiatric Genomics Consortium and UK Biobank. The inverse-variance weighted method was used to estimate the association of genetically proxied morning diurnal preference, corresponding to a 1-hour earlier sleep midpoint, with MDD risk.
Exposures: Morning diurnal preference scaled to a 1-hour earlier, objectively measured sleep midpoint.
Main outcomes and measures: Risk of MDD, including self-reported and clinically diagnosed cases, as ascertained in meta-analyses of genome-wide association studies.
Results: A total of 697 828 individuals (all of European ancestry) were in the UK Biobank and 23andMe cohorts; 85 502 in the UK Biobank had measurements of the sleep midpoint. A further 170 756 individuals with MDD and 329 443 control participants (all of European ancestry) were in the Psychiatric Genomics Consortium and UK Biobank data. Genetically proxied earlier diurnal preference was associated with a 23% lower risk of depression (odds ratio [OR] per 1-hour earlier sleep midpoint, 0.77 [95% CI, 0.63-0.94]; P = .01). This association was similar when restricting analysis to individuals with MDD as stringently defined by the Psychiatric Genomics Consortium (OR, 0.73 [95% CI, 0.54-1.00]; P = .05) but not statistically significant when defined by hospital-based billing codes in the UK Biobank (OR, 0.64 [95% CI, 0.39-1.06]; P = .08). Sensitivity analyses examining potential bias due to pleiotropy or reverse causality showed similar findings (eg, intercept [SE], 0.00 [0.001]; P = .66 by Egger intercept test).
Conclusions and relevance: The results of this mendelian randomization study support a protective association of earlier diurnal preference with risk of MDD and provide estimates contextualized to an objective sleep timing measure. Further investigation in the form of randomized clinical trials may be warranted.